Thyroid function tests
| Thyroid function tests | |
|---|---|
| Intervention | |
| MeSH | D013960 |
Thyroid function tests (TFTs) is a collective term for blood tests used to check the function of the thyroid.[1]
TFTs may be requested if a patient is thought to suffer from hyperthyroidism (overactive thyroid) or hypothyroidism (underactive thyroid), or to monitor the effectiveness of either thyroid-suppression or hormone replacement therapy. It is also requested routinely in conditions linked to thyroid disease, such as atrial fibrillation and anxiety disorder.
A TFT panel typically includes thyroid hormones such as thyroid-stimulating hormone (TSH, thyrotropin) and thyroxine (T4), and triiodothyronine (T3) depending on local laboratory policy.
Contents |
Thyroid hormones
Thyroid-stimulating hormone
Thyroid-stimulating hormone (TSH, thyrotropin) is generally elevated in hypothyroidism and decreased in hyperthyroidism.[2]
| Patient type | Lower limit | Upper limit | Unit |
| Adults - standard range |
0.3[3], 0.4[4], 0.5[5], 0.6[6] | 3.0 , 4.0[3], 4.5[4], 6.0[5] | mIU/L or μIU/mL |
| Adults - optimal range |
0.3[7] , 0.5[8] | 2.0[8] , 3.0[7] | mIU/L or μIU/mL |
| Infants | 1.3[9] | 19[9] | mIU/L or μIU/mL |
Total thyroxine
Total thyroxine (Total T4) is generally elevated in hyperthyroidism and decreased in hypothyroidism.[2] It is usually slightly elevated in pregnancy secondary to increased levels of thyroid binding globulin (TBG).[2]
Reference ranges:
| Lower limit | Upper limit | Unit |
| 4[10], 5.5[4] | 11[10], 12.3[4] | μg/dL |
| 60[10][11] | 140[10], 160[11] | nmol/L |
Free thyroxine
Free thyroxine (Free T4) is generally elevated in hyperthyroidism and decreased in hypothyroidism.[2]
| Patient type | Lower limit | Upper limit | Unit |
| Normal adult | 0.7[12] ,0.8[4] | 1.4[12], 1.5[4], 1.8[13] | ng/dL |
| 9[14][3], 10[10], 12 [11] | 18[3][14] , 23[11] | pmol/L | |
| Infant 0–3 d | 2.0[12] | 5.0[12] | ng/dL |
| 26[14] | 65[14] | pmol/L | |
| Infant 3–30 d | 0.9[12] | 2.2[12] | ng/dL |
| 12[14] | 30[14] | pmol/L | |
| Child/Adolescent 31 d – 18 y |
0.8[12] | 2.0[12] | ng/dL |
| 10[14] | 26[14] | pmol/L | |
| Pregnant | 0.5[12] | 1.0[12] | ng/dL |
| 6.5[14] | 13[14] | pmol/L |
Total triiodothyronnine
Total triiodothyronine (Total T3) is generally elevated in hyperthyroidism and decreased in hypothyroidism.[2]
Reference ranges:
| Test | Lower limit | Upper limit | Unit |
| Total triiodothyronine | 60[4], 75[10] | 175[10], 181[4] | ng/dL |
| 0.9[3] , 1.1[10] | 2.5[3] , 2.7[10] | nmol/L |
Free triiodothyronnine
Free triiodothyronine (Free T3) is generally elevated in hyperthyroidism and decreased in hypothyroidism.[2]
Reference ranges:
| Patient type | Lower limit | Upper limit | Unit |
| Normal adult | 0.2[10] | 0.5[10] | ng/dL |
| 3.1[15] | 7.7[15] | pmol/L | |
| Children 2–16 y | 0.1[16] | 0.6[16] | ng/dL |
| 1.5[15] | 9.2[15] | pmol/L |
Calculated indices of free hormones
- Free T4 index
- Free T3 index
Carrier proteins
Thyroxine-binding globulin
An increased thyroxine-binding globulin results in an increased total thyroxine and total triiodothyronine without an actual increase in hormonal activity of thyroid hormones.
Reference ranges:
| Lower limit | Upper limit | Unit |
| 12[4] | 30[4] | mg/L |
Thyroglobulin
Reference ranges:
| Lower limit | Upper limit | Unit |
| 1.5[10] | 30[10] | pmol/L |
| 1[10] | 20 [10] | μg/L |
Other binding hormones
- Transthyretin (prealbumin)
- Albumin
Protein binding function
Thyroid hormone uptake
Thyroid hormone uptake (Tuptake or T3 uptake) is a measure of the unbound thyroxine binding globulins in the blood, that is, the TBG that is unsaturated with thyroid hormone.[2] Unsaturated TBG increases with decreased levels of thyroid hormones. It is not directly related to triiodothyronine, despite the name T3 uptake.[2]
Reference ranges:
| Patient type | Lower limit | Upper limit | Unit |
| Females | 25[2] | 35[2] | % |
| In pregnancy | 15[2] | 25[2] | % |
| Males | 25[2] | 35[2] | % |
Other protein binding tests
- Thyroid hormone binding ratio (THBR)
- Thyroxine-binding index (TBI)
Mixed parameters
Free thyroxine index
The Free Thyroxine Index (FTI or T7) is obtained by multiplying the total T4 with Tuptake.[2] FTI is considered to be a more reliable indicator of thyroid status in the presence of abnormalities in plasma protein binding.[2]
FTI is elevated in hyperthyroidism and decreased in hypothyroidism.[2]
| Patient type | Lower limit | Upper limit | Unit |
| Females | 1.8[2] | 5.0[2] | |
| Males | 1.3[2] | 4.2[2] |
Structure parameters
For special purposes, e.g. in diagnosis of nonthyroidal illness syndrome or central hypothyroidism, derived structure parameters that describe constant properties of the overall feedback control system, may add useful information.[17][18]
Secretory capacity (GT)
Thyroid's secretory capacity (GT) is the maximum stimulated amount of thyroxine the thyroid can produce in one second.[19] GT is elevated in hyperthyroidism and reduced in hypothyroidism.[20]
GT is calculated with
![\hat G_T = {{\beta _T (D_T %2B [TSH])(1 %2B K_{41} [TBG] %2B K_{42} [TBPA])[FT_4 ]} \over {\alpha _T [TSH]}}](/2012-wikipedia_en_all_nopic_01_2012/I/d85f820cf6d8564e68ea2e1e953d34e4.png)
or
![\hat G_T = {{\beta _T (D_T %2B [TSH])[TT_4 ]} \over {\alpha _T [TSH]}}](/2012-wikipedia_en_all_nopic_01_2012/I/85f4ffe767159d3e591b02fa2b6cfea6.png)
 : Dilution factor for T4 (reciprocal of apparent volume of distribution, 0.1 l-1)
: Dilution factor for T4 (reciprocal of apparent volume of distribution, 0.1 l-1)
 : Clearance exponent for T4 (1.1e-6 sec-1)
: Clearance exponent for T4 (1.1e-6 sec-1)
K41: Dissociation constant T4-TBG (2e10 l/mol)
K42: Dissociation constant T4-TBPA (2e8 l/mol)
DT: EC50 for TSH (2.75 mU/l)[19]
| Lower limit | Upper limit | Unit |
| 1.41[19] | 8.67[19] | pmol/s |
Web Link
SPINA Thyr: Open source software for calculating GT and GD
Sum activity of peripheral deiodinases (GD)
The sum activity of peripheral deiodinases (GD) is reduced in nonthyroidal illness with hypodeiodination.[18]
GD is obtained with
![\hat G_D = {{\beta _{31} (K_{M1} %2B [FT_4 ])(1 %2B K_{30} [TBG])[FT_3 ]} \over {\alpha _{31} [FT_4 ]}}](/2012-wikipedia_en_all_nopic_01_2012/I/621776f15f079ad79da1f8a9c4ce9961.png)
or
![\hat G_D = {{\beta _{31} (K_{M1} %2B [FT_4 ])[TT_3 ]} \over {\alpha _{31} [FT_4 ]}}](/2012-wikipedia_en_all_nopic_01_2012/I/60a26cf9a1d8e02229bc75bc4f3d5832.png)
 : Dilution factor for T3 (reciprocal of apparent volume of distribution, 0.026 l-1)
: Dilution factor for T3 (reciprocal of apparent volume of distribution, 0.026 l-1)
 : Clearance exponent for T3 (8e-6 sec-1)
: Clearance exponent for T3 (8e-6 sec-1)
KM1: Dissociation constant of type-1-deiodinase (5e-7 mol/l)
K30: Dissociation constant T3-TBG (2e9 l/mol)[19]
| Lower limit | Upper limit | Unit |
| 20[19] | 40[19] | nmol/s |
Web Link
SPINA Thyr: Open source software for calculating GT and GD
TSH index
TSH index (TSHI) helps to determine thyrotropic function of anterior pituitary on a quantitative level.[21]
It is calculated with
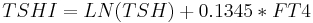 .
.
Additionally, a standardized form of TSH index may be calculated with
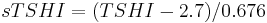 .[21]
.[21]
| Parameter | Lower limit | Upper limit | Unit |
| TSHI | 1.3[21] | 4.1[21] | |
| sTSHI | -2[21] | 2[21] |
See also
References
- ^ Dayan CM (February 2001). "Interpretation of thyroid function tests". Lancet 357 (9256): 619–24. doi:10.1016/S0140-6736(00)04060-5. PMID 11558500. http://linkinghub.elsevier.com/retrieve/pii/S0140-6736(00)04060-5.
- ^ a b c d e f g h i j k l m n o p q r s t u Military Obstetrics & Gynecology > Thyroid Function Tests In turn citing: Operational Medicine 2001, Health Care in Military Settings, NAVMED P-5139, May 1, 2001, Bureau of Medicine and Surgery, Department of the Navy, 2300 E Street NW, Washington, D.C., 20372-5300
- ^ a b c d e f Reference range list from Uppsala University Hospital ("Laborationslista"). Artnr 40284 Sj74a. Issued on April 22, 2008
- ^ a b c d e f g h i j Normal Reference Range Table from The University of Texas Southwestern Medical Center at Dallas. Used in Interactive Case Study Companion to Pathologic basis of disease.
- ^ a b Blood Test Results - Normal Ranges Bloodbook.Com
- ^ The TSH Reference Range Wars: What's "Normal?", Who is Wrong, Who is Right... By Mary Shomon, About.com. Updated: June 19, 2006. About.com Health's Disease and Condition
- ^ a b 2006 Press releases: Thyroid Imbalance? Target Your Numbers Contacts: Bryan Campbell American] Association of Clinical Endocrinologists
- ^ a b The TSH Reference Range Wars: What's "Normal?", Who is Wrong, Who is Right... By Mary Shomon, About.com. Updated: June 19, 2006
- ^ a b Demers, Laurence M.; Carole A. Spencer (2002). "LMPG: Laboratory Support for the Diagnosis and Monitoring of Thyroid Disease". National Academy of Clinical Biochemistry (USA). http://www.nacb.org/lmpg/thyroid_LMPG_PDF.stm. Retrieved 2007-04-13. — see Section 2. Pre-analytic factors
- ^ a b c d e f g h i j k l m n o Table 4: Typical reference ranges for serum assays - Thyroid Disease Manager
- ^ a b c d van der Watt G, Haarburger D, Berman P (July 2008). "Euthyroid patient with elevated serum free thyroxine". Clin. Chem. 54 (7): 1239–41. doi:10.1373/clinchem.2007.101428. PMID 18593963. http://www.clinchem.org/cgi/content/full/54/7/1239.
- ^ a b c d e f g h i j Free T4; Thyroxine, Free; T4, Free UNC Health Care System
- ^ Derived from molar values using molar mass of 776.87 g/mol
- ^ a b c d e f g h i j Derived from mass values using molar mass of 776.87 g/mol
- ^ a b c d Derived from mass values using molar mass of 650.98 g/mol
- ^ a b Cioffi M, Gazzerro P, Vietri MT, et al. (2001). "Serum concentration of free T3, free T4 and TSH in healthy children". J. Pediatr. Endocrinol. Metab. 14 (9): 1635–9. PMID 11795654.
- ^ Dietrich, J. W., A. Stachon, B. Antic, H. H. Klein, and S. Hering (2008). "The AQUA-FONTIS Study: Protocol of a multidisciplinary, cross-sectional and prospective longitudinal study for developing standardized diagnostics and classification of non-thyroidal illness syndrome." BMC Endocrine Disorders 8 (13). PMID 18851740.
- ^ a b Rosolowska-Huszcz D, Kozlowska L, Rydzewski A (2005). Influence of low protein diet on nonthyroidal illness syndrome in chronic renal failure. Endocrine. 27(3):283-8. PMID 16230785
- ^ a b c d e f g Dietrich, J. W. (2002), Der Hypophysen-Schilddrüsen-Regelkreis, Berlin, Germany: Logos-Verlag Berlin, ISBN 978-3-89722-850-4, OCLC 50451543, 3897228505, http://openlibrary.org/books/OL24586469M/Der_Hypophysen-Schilddrüsen-Regelkreis
- ^ Dietrich, J., M. Fischer, J. Jauch, E. Pantke, R. Gärtner und C. R. Pickardt (1999). "SPINA-THYR: A Novel Systems Theoretic Approach to Determine the Secretion Capacity of the Thyroid Gland." European Journal of Internal Medicine 10, Suppl. 1 (5/1999): S34.
- ^ a b c d e f Jostel A, Ryder WD, Shalet SM. The use of thyroid function tests in the diagnosis of hypopituitarism: definition and evaluation of the TSH Index. Clin Endocrinol (Oxf). 2009 Oct;71(4):529-34. PMID 19226261.
|
||||||||||||||||||||||||||||||||||